Carpal Tunnel
- related: MSK
- tags: #msk
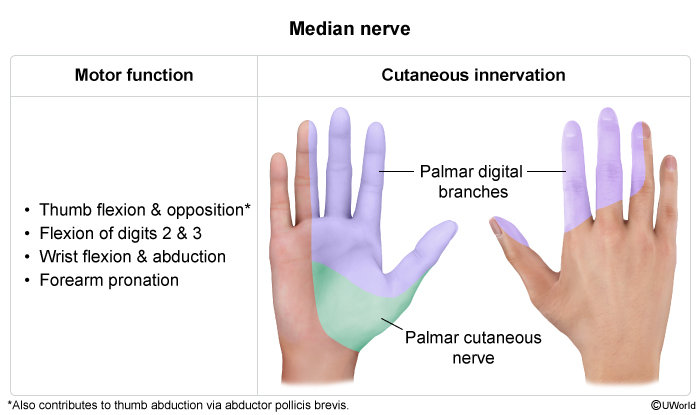
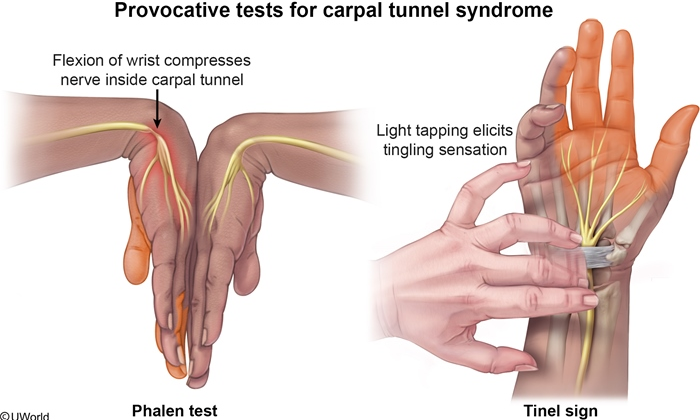
Symptoms of CTS are frequently worse at night and can be exacerbated by repetitive/sustained hand movements (eg, knitting). Preservation of sensation over the thenar eminence is highly indicative as the palmar sensory cutaneous branch of the median nerve goes over, not through, the carpal tunnel. Provocative maneuvers such as the Phalen and Tinel tests have limited sensitivity (~60%) and specificity (~70%).
CTS is primarily a clinical diagnosis. Nerve conduction studies (NCS) are usually performed during atypical presentations, to evaluate disease severity, and prior to considering surgery (sensitivity 56%-85%, specificity 94%). Electromyography is often done with NCS to differentiate neurogenic versus myopathic weakness. Neither of these studies is necessary in this patient as her symptoms are mild and her presentation is typical of CTS (Choice C).
Compression of the median nerve in carpal tunnel syndrome (CTS) results in loss of myelination. Axonal loss may also occur if the compression is severe. Nerve conduction studies (NCS) can confirm the diagnosis and assess the severity of CTS by demonstrating slowed conduction along the nerve at the level of the carpal tunnel. Reduced amplitudes indicate axonal loss. Electromyography (EMG) is frequently combined with NCS and may show denervation of muscles innervated by the median nerve with relative sparing of those that are not.
NCS and EMG are indicated for patients with chronic or refractory CTS who are being considered for surgery. They are not usually needed in the initial diagnosis (which is typically based on clinical features) but can be considered if the diagnosis is uncertain.
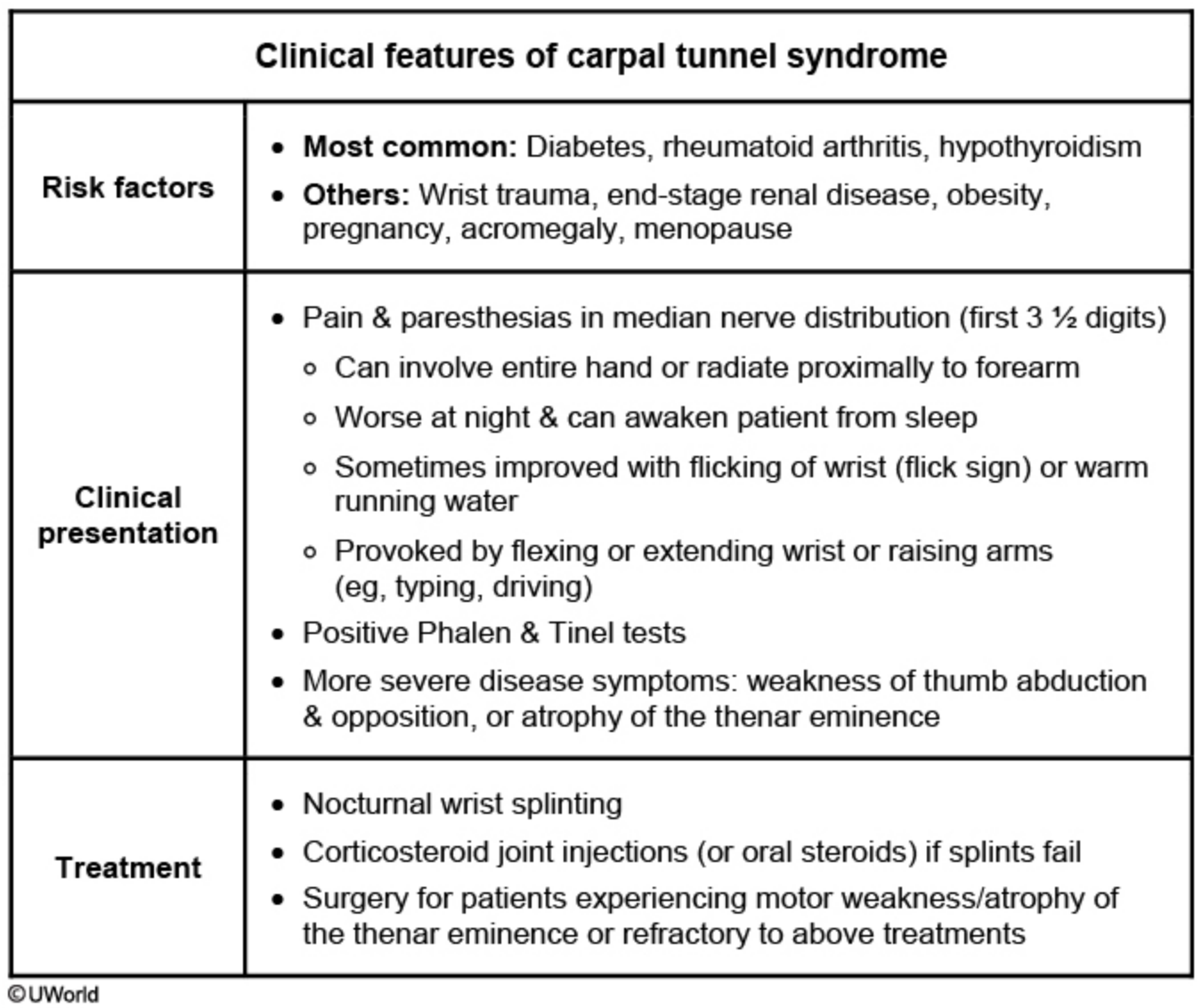
This patient's presentation is consistent with carpal tunnel syndrome (CTS) with severe right median neuropathy across the wrist. Mild to moderate CTS typically presents with intense wrist pain without hand muscle weakness, atrophy, or obvious EMG evidence of median nerve axonal injury. Most patients with mild to moderate CTS respond to conservative therapy (e.g., wrist splint, steroid injections). Nocturnal wrist splinting keeps the wrist in a neutral position to improve flexion and extension, and is preferred initially in most patients. Patients who do not respond to wrist splinting may be treated with wrist glucocorticoid injections. Patients who refuse injections can be treated with a short course of oral steroids. It is important to remember that steroid injections provide only short-term symptomatic relief (1 to 3 months).
Surgical median nerve decompression is recommended for patients with severe symptoms (or evidence of axonal injury on EMG) or mild to moderate symptoms refractory to conservative therapy.